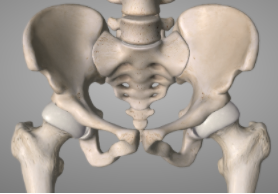
As a structure the pelvis provides a link between the trunk and legs. It can be thought of as a stable base for the trunk to move on, and a stable platform for the legs to create force and motion through. Essentially, the pelvis functions to transmit force between the legs and trunk.
FACTS:
- There are three joints that make up the pelvis, two sacroiliac joints at the back and the pubic symphysis at the front.
- The pelvic joints are designed for load transfer and are inherently stable.
- Approximately 65% of body weight is transmitted through the sacrum and into the lower back when standing.
- The pelvis has a similar pain pattern as the lower back. It is estimated that the sacroiliac joint is causing pain in 20-25% of people diagnosed with non-specific lower back pain.
ANATOMY OF THE PELVIS:
- The pelvis has two joints at the back, the sacroiliac joints, which are the joints between the sacrum and ilium.
- The pubic symphysis is the ligament that spans between the two pubic bones at the front.
- There are also the hip joints, which is where the femur articulates with the pelvis.
- The lumbar spine then also attaches to the sacrum posteriorly
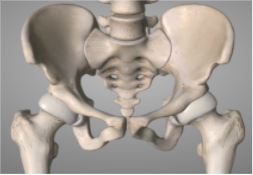
As we add the ligaments and the muscles to the pelvis, it becomes apparent how complex and intricate the pelvis is. The ligaments and muscles work together with the unique shape of the bones of the pelvis to create an inherently stable ‘base’.
See below:
- Posterior view of the pelvis including ligaments
- Posterior view of the pelvis with stabilising muscles and ligaments included.
- Posterior view of pelvis with all muscles included. Note that there is almost no aspect of the pelvic bones that are exposed

HOW DOES THE PELVIS WORK?
Different to most other joints in the body, the joints of the pelvis are designed to be stiff, stable and have very little movement; in fact, there is only 2-5° of movement at these joints. This movement is controlled during load transfer (ie. walking) by engaging stabilising muscles which assist in tensioning the ligaments that cross the pelvic joints. As you can see from the pictures above, there are many muscles that must work in a coordinated fashion to enable effective load transfer.
WHY DO I HAVE PELVIC PAIN?
Pelvic pain generally occurs as a result of a change in the pattern of muscle activation. The altered coordination of muscles can be the primary or secondary factor. This means either the altered muscle activation is primarily causing pain; or, the altered activation is a secondary response to something else (ie. a lower back injury) that then changes patterns of muscle activation. This altered muscle activation then affects the ability of the pelvis to transfer load. Generally, this occurs secondary to;
- Pregnancy (please click here to go to the pregnancy-related pelvic girdle pain blog).
- A change in biomechanics that affect the loading pattern of the pubic symphysis or sacroiliac joints; for example, work or sport that places a significant load on one side more than the other.
- An imbalance or altered activation of the lumbopelvic muscles.
- An injury ie. significant fall or accident.
When assessing the pelvis, we also have to include the hips, lower back and the upper trunk (thoracic spine, ribcage, diaphragm etc). With consideration of these joints, we also must consider the 35+ muscles that attach directly to the pelvis.
WHAT CAN I DO ABOUT MY PELVIC PAIN?
As with any injury, the most important aspect of managing pelvic pain is obtaining an accurate diagnosis. Majority of people who present with pelvic pain will have a significant ‘driver’ which has either caused or contributed to their symptoms developing. Establishing what the driver is and how to best manage it is essential to effectively treat pelvic pain.
WHAT WILL MY TREATMENT LOOK LIKE?
At The Injury Clinic, our management plan will focus on:
- Establishing a diagnosis and understanding of the cause (or driver) of your pelvic pain,
- Starting treatment, which may include;
- Manual therapies,
- Strengthening and retraining exercises,
- Pelvic support belts or tape (if indicated and appropriate).
- Re-introducing or establishing a plan to maintain activity and load,
- Increasing strength in the appropriate muscle groups.
IN SUMMARY
The pelvis can be a complicated area of the body to treat as there are so many different factors that contribute to the development of pain and injury. At The Injury Clinic, we complete an extensive assessment to ensure we correctly identify these contributing factors and can establish an effective treatment plan. If you would like more information, please do not hesitate to call us on (03) 5229 3911 or email us info@theinjuryclinic.com.au.